Factsheet and FAQ’s on Hypospadias
Hypospadias is a very common congenital anomaly, which requires surgical correction. The incidence of this condition is 1 in 250 to 300 live births
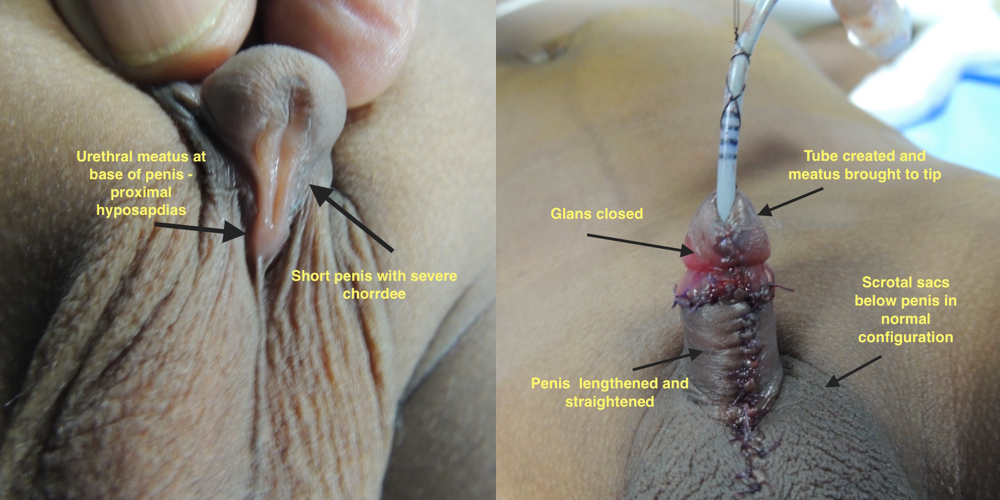
This condition happens in male children when the urinary opening is not on the tip of the penis but on the bottom (ventral) surface
Hypospadias may be associated with a bend (chordee) and poor penile development
Surgical correction is aimed at # correcting the bend to enable a straight penis for satisfactory sexual intercourse # bringing the urinary orifice to the tip of the penis so that urine can be passed standing and in a straight stream away from the body
There are very many grades of hypospadias but a very simple way of looking at the problem will be to assess where the abnormal urinary opening is located – near the tip (distal), on the shaft (mid), at the base (proximal), in between the scrotal sacs (perineal). As a general rule the more the shaft moves to the base of the penis the more severe the chordee
Two Years After Hypospadias Repair

Now for some FAQ’s
When should I get my child operated?
Ideally before one year of age. The reasons for this are pretty straightforward. At this age children are not ambulant and can easily be pacified looked after. The older the child the greater is the difficulty in managing the child in the postoperative period. Again when done early the memory of surgery on the genitalia is not retained.
What exactly is done at surgery? Will you create a urine tube with a foreign substance?
The first aim at surgery is correcting the bend in the penis and ensuring it is straight with an‘artificial erection test’ on the operating table. The second step is to make a tube which can conduct urine – this is made from the child’s own tissues. Thirdly the tip of the penis is shaped (Glansplasty). Fourthly the skin is readjusted to give a normal appearance. Ideally after hypospadias repair it should like as if a circumcision has been done. However if the parents are particular and if the excess skin will permit a normal foreskin (uncircumcised appearance) can be created.
After such major surgery will the child be in a lot of pain? How will we manage him? How will he pass urine?
Pain management is part of anesthestia. The team will ensure that the child is pain free and comfortable. Urine will be passed in a tube kept inside his penis. It will either drain into a diaper (which needs to be changed periodically) or will drain into a bag (which needs to be emptied)
When will the bandages come off and when can I see my son pass urine normally?
Usually the bandages are removed 5 – 7 days after surgery. In apprehensive children a mild sedative or anesthesia is given to remove the bandages. There will be a tube in the penis which will be removed a week to ten days after the procedure. The removal of this tube is done in the outpatient clinic and is a painless procedure.
What sort of complications can I expect?
There are many complications in hypospadias repair. The commonest is a leak from urethral tube – usually these settle within six months. Other issues are narrowing of the new opening at the tip of the penis, a narrowing (stenosis) of the tube, sutures on the glans giving way (dehiscence) or necrosis of the skin used to cover the penis. This is by no means an exhaustive list of complications but only indicative of the commoner ones.
Do complications mean more surgery can be expected?
Generally yes. In every case the surgeon will tell you the numbers he does every year and his own complication rate. Usually a fistula rate of around 10 – 30 % can be expected even in expert hands.
The surgeon told me the repair cannot be completed in one stage – what does this mean?
It means the problem is severe and will require two stages or more for full correction. In a staged repair the following steps are usually done:
Stage 1 – Correction of the chordee and rearrangement of skin
Stage 2 – Creation of a tube and shaping the tip of the penis (glans plasty). This is usually done six months after stage 1.
Stage 3 – Rearrangement of scrotal sacs so that they hang below the penis and not float above it. This stage is required only in a small minority with very severe (perineal) hypospadias.
My surgeon has arranged for a consultation with a pediatric endocrinologist? Is it necessary?
Sometimes when the penis is very small the surgeon may request the pediatric endocrinologist to see the child and run some tests to make sure male hormonal production is OK. In the same vein if the head of the penis (called glans penis) is very small, hormonal injections may be prescribed to increase the size before surgery.
Can the glans penis be closed normally in every case? My surgeon says it may not be possible?
In very proximal hypospadias the glans may be so small that it just be impossible to close it over the urethral tube to give a normal appearance. However even in this case the urethra can be brought to the tip of the penis to enable a normal stream of urine to be passed.
How long do I need to followup? What if my child has problems at puberty?
Your surgeon will give a regular schedule of followup visits upto puberty and beyond to ensure that 1. minor problems are taken care of and 2. proper growth, development and cosmetic appearance is ensured so that the child grows up to be a confident adult.
Our unit at Apollo Children’s Hospital does more than 120 complex hypospadias repairs every year. These include primary and redo-repairs.
We have a complication rate of around 15%. Most complications are minor wound breakdowns and small fistulae (which heal spontaneously). This complication rate is within the acceptable range considering the large number of proximal hypospadias and redo procedures that we do regularly.